A Neurodivergent Manifesto from the Edges of the NHS
By Thomas Delahunt & Matt Taiano
“What the caterpillar calls the end of the world, the master calls a butterfly.”
— Richard Bach
This piece forms part of an unfolding conversation now hosted at
🔗 thomasdelahunt.substack.com
—a home for poetic resistance, neurodivergence, and the red thread of becoming.
1. The Poetic Nursing Heartbeat
This piece lives within the Poetic Nursing Heart—a rhythm that began over five years ago and still beats today. It was born from rupture, grief, absurdity, and an impossible tenderness we call nursing.
Now, its pulse has grown louder.
We, Thomas and Matt, both began our careers in emergency nursing. One still deep in the system, the other walking its poetic perimeter. We share a professional kinship, yes—but also something deeper: a trauma-bonded knowing that comes from surviving inside systems that heal others but sometimes forget their healers, especially those hidden behind masks.
This piece is our heart song.
It’s a pulse returned.
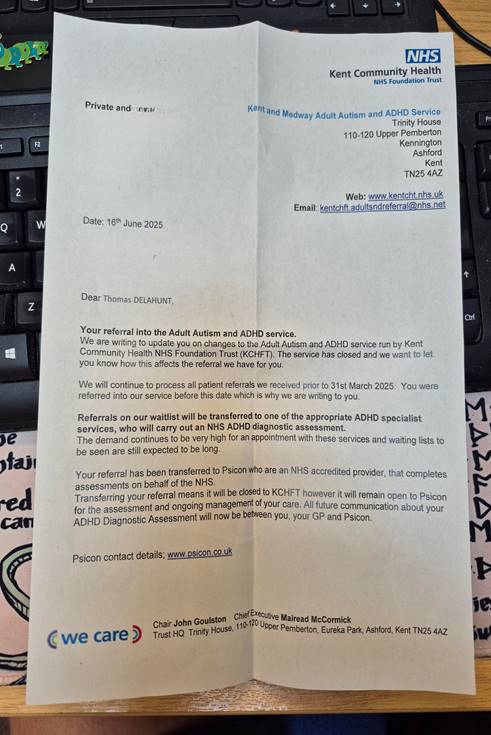
The Collapse is Quiet
On 16th June 2025, a letter arrived. Official. Unremarkable.
It said the neurodevelopmental service I was referred to—five years ago—was now closed.
No apology. No options.
Just… gone.
But the collapse it sparked wasn’t visible.
I am trained to present well.
It was internal. It folded in on sleep, memory, food, trust.
It rewired my nervous system in subtle, destabilising ways.
I did not scream.
I simply stayed——waiting, watching, whispering.
Trauma-Bonded: The Hidden Currents in Nursing
There’s a word for what many of us live through: trauma bonding. Once reserved for personal relationships, it now appears in studies of moral injury and collective distress in healthcare (Smith & Freyd, 2014; Burgess et al., 2020).
Nurses don’t just work together—we survive together.
We pass one another in corridors, in post-codes, in held-back tears and dark humour. We meet not in joy but in collapse.
And that becomes identity.
“We are raised in crisis,” Matt writes.
“We build trust from adrenaline, and intimacy from exhaustion.”
Entangled Minds, Poetic Brains
I don’t read conventionally.
I don’t write conventionally.
But I see things. Systems. Shapes. Wounds. Waves.
My mind is not disordered—it’s entangled.
I move in loops, not lines.
I learn like a forest learns: through pattern, resonance, rupture.
I have long walked with Spinoza, Camus, Jung, Goethe, Schopenhauer.
Not academically—but psychically.
They form a constellation of insight that helps me interpret pain and possibility.
But our systems ask for something else. Something standard.
And that’s where many of us fall through.
Neurodivergent Nurses: The Unseen Workforce
In 2023, a Freedom of Information request confirmed that over 150,000 people are on neurodevelopmental assessment waitlists in England. But that figure hides what we know intuitively: most nurses never even enter the queue.
We don’t trust the system.
We’re afraid of reprisal.
We’re too burned out to fill in another form.
And yet we carry ADHD, autism, dyslexia, CPTSD—in silence.
Behind name badges. Under clipboards.
“This isn’t about accommodation,” Matt says.
“It’s about recognition. We are already here. Already working. Already holding the NHS together.”
The Table of Consciousness
From this quiet breakdown came a project:
The Table of Consciousness—a co-authored proposal for radical diagnostic culture and poetic assessment.
It has been submitted to Arts Council England and will live as an installation, a dialogue space, and a place of embodied listening. It will also form part of my PhD submission—where arts-based methodologies intersect with trauma-informed practice and poetic research.
This is not a call for pity.
It is a proposal—to redesign our systems in the image of our most silenced carers.
Matt’s insight is foundational to this.
As a specialist nurse in neurodivergent pathways, he brings not just knowledge—but witness.
We build this table together.
The Heart Song
The Poetic Nursing Heart has always been more than metaphor. It is our metronome.
It beats with pain, absurdity, laughter, grief, and grit. This piece is its new stanza.
A manifesto. A murmuration. A beginning again. From emergency room to writing room.
From burnout to blueprint. From whisper to voice.
A Simple Poem
The whispers are finally heard.
The waiting room held its breath,
Five years, folded into silence.
A letter fell, like a leaf from a tired tree.
We turned, not away—but toward.
And the whispers became voice.

Matt’s Voice: From Burnout to Advocacy;
I have been an RGN at my trust since 2013, having trained at CCCU from 2010. My background is in critical care nursing, and I currently work as a Band 7 Resus Officer.
I’ve always felt different. Anxious. The odd one out.
In 2009, while training as a teacher, I was diagnosed with dyslexia. University was supportive, and I completed my BSc in Adult Nursing. But in clinical practice, the feelings of not fitting in persisted. I often felt “stupid,” “needy,” and like a burden—to peers, to the team, to myself.
In 2022, I began a Band 6/7 development role as a Resus Officer. From the start, I knew it wasn’t a good fit. I failed to meet my probation KPIs, mostly around admin, and was put on a performance plan—despite waiting for Access to Work support for my dyslexia.
Without support, I spiralled. I was exhausted and lost. Eventually, I took 12 weeks off with severe anxiety, depression, and burnout. The RCN supported me through a formal grievance, and it was agreed that performance management was inappropriate given my neurodivergent needs. The previous actions were rescinded, and I was promoted to Band 7 with proper support.
Then, life collapsed again: three family deaths in six months. I became overwhelmed. The fog returned. So did the deep sense of being different, misunderstood, broken.
That’s when I sought further assessment. I was diagnosed with ADHD (mixed presentation), and a consultant psychiatrist said I also met the criteria for autism, though she couldn’t formally diagnose it. Through “Right to Choose,” I pursued an ASD assessment, but the service closed. I received a letter saying it wouldn’t happen.
Still, I’m now medicated for ADHD—which helps—and I receive coaching from a neurodivergent job coach. We speak about perception, stress, identity. It grounds me.
My employer—one of the largest trusts in the country—tries. But it isn’t enough. Staff are not protected. They are not understood. They are burning out.
So I did something: I created a Facebook group for neurodivergent NHS staff and allies. No bands. No uniforms. Just safety. We began in January 2024 with 15 members. As of now, we’re at 315.
The message is clear: current support is not enough.
Since founding the group, I’ve been invited to become a Staff Governor, present to the Trust Board, deliver training to senior leaders, and mentor students in ways that honour their neurodivergence.
Through this work, I connected with Tom—a fellow ND voice and a lecturer at CCCU. Together, we’re pushing forward.
We are not broken. We are not burdens. We are part of the future of healthcare.
We want to be seen, supported, and celebrated.
I don’t want to be placed on a pedestal. I just want to help people without having to hide who I am. I want to be part of a workforce where difference is recognised as strength—and where healing is possible for us, too
From Trauma Bond to Collective Voice: A Call to the NHS leaders…
………
We, Thomas and Matt, are two nurses bound not just by profession, but by a deep, unspoken trauma bond—one forged in the quiet collapse of trying to survive within a system that often forgets its healers. Our neurodivergence—ADHD, dyslexia, possible autism—has shaped our experience, but for too long, it remained unseen, unsupported, and misunderstood.
What we share is not unique. Behind clipboards and compassion, many nurses are masking burnout, anxiety, and difference. We know this not just from data—but from our own bodies, our own breakdowns.
We are not asking for pity.
We are asking for recognition, for representation, and for real conversation.
This is a call to all those working in or alongside the NHS:
Join us.
Talk with us.
Help build spaces where neurodiverse nurses are no longer silent, no longer sidelined, and no longer surviving in isolation.
Together, let’s shift the culture—from burnout to belonging.
Let’s redesign the system in the image of its most silenced carers.
Reach out.
Listen deeply.
Let the heart lead.
References
- Burgess, M., Irvine, F., & Wainwright, P. (2020). An exploration of moral injury in the nursing workforce. Nursing Ethics, 27(3), 932–945.
- Smith, C. P., & Freyd, J. J. (2014). Institutional betrayal. American Psychologist, 69(6), 575–587.
- Young, S., Asherson, P., Lloyd, T., & Absoud, M. (2021). Diagnosing ADHD in Adults: An Update on the Evidence. BMJ, 374:n698.
- McVicar, A. (2016). Scoping the common antecedents of job stress and job satisfaction for nurses. International Journal of Nursing Studies, 52(2), 637–650.
Join the rhythm. The heart still beats.
 The Poetic Nursing Heart
The Poetic Nursing Heart Tom Delahunt
Tom Delahunt 1722
1722